IPFCC provides essential leadership for advancing the practice of patient- and family-centered care. By promoting collaborative, empowering partnerships among patients, families, and health care professionals, IPFCC facilitates patient- and family-centered change in all health care settings
Below is a selection of projects completed over the last decade:
Texas Collaborative for Healthy Mothers and Babies
IPFCC served as a subcontractor to assist TCHMB with building capacity to advance a culture of health equity in their perinatal quality care collaborative’s work. IPFCC worked closely with the TCHMB team throughout this project to incorporate actionable steps to engage clinicians, midwives, doulas, patients, and families and develop partnerships to enhance equitable, quality, and respectful care for mothers and babies in Texas.
Patient- and Family-Centered Care and Pediatric Partnerships During COVID-19
Funded by a grant from the Lucile Packard Foundation for Children’s Health, Palo Alto, California, IPFCC led a six-month project to serve as a resource to provide up-to-date, easily accessible, information to children’s hospitals and other pediatric programs about ways to stay grounded in PFCC core concepts during COVID-19. A series of free webinars and online conversations occurred monthly from May through October 2020 on topics including vulnerable children and children’s mental health needs. These learning events highlighted initiatives in the field in response to the pandemic that were planned and conducted in partnership with patient and family advisors.

Amplifying the Peer Voice in Behavioral Health Research to Drive Transformation
IPFCC, in partnership with the Depression and Bipolar Support Alliance (DBSA), is leading a project that will build a better understanding of peer priorities for behavioral health research and promote collaborative relationships between clinicians/researchers and individuals with lived experience of mood disorders. This project is funded by a Eugene Washington Engagement Award from the Patient-Centered Outcomes Institute Research (PCORI). A centerpiece of this project is a virtual convening that will bring together various stakeholders to share information about research on mood disorders, discuss future research priorities, and develop collaborative relationships among participants.

Moving Forward with Patient- and Family-Centered Care: Partnerships for Quality and Safety
Almost 200 participants, including 35 patient and family advisors, gathered in Detroit on June 13-14, 2019 to expand their knowledge of patient- and family-centered care. They came from across the U.S., Canada, the Netherlands and the United Arab Emirates. Included among the participants were teams representing 69 health care organizations. Leadership support for this intensive seminar was provided by the MHA Keystone Center of the Michigan Health & Hospital Association and Beaumont Health, the largest health system in Michigan.
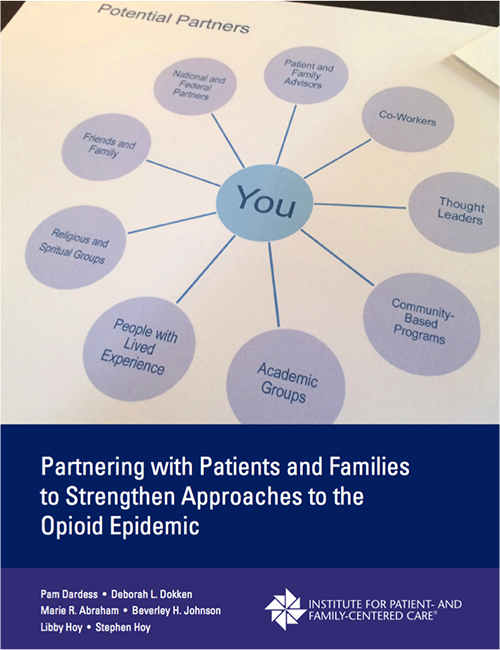
Patient and Family Advisor (PFA) Summit on the Opioid Epidemic
In June 2018, IPFCC and PFCCpartners hosted a Patient and Family Advisor (PFA) Summit on the Opioid Epidemic. Sponsored by Beaumont Health, the PFA Summit was attended by more than 80 participants—over half of whom were patient and family advisors. Participants discussed how to apply the core concepts of patient- and family-centered care to the opioid epidemic, and identified ways in which they could contribute to partnerships and solutions moving forward. In November 2018, IPFCC released a White Paper, co-authored with PFCCpartners, which builds upon the presentations and discussions from the Summit and makes recommendations to further strengthen collaboration with patients and families, especially those with lived experience.

8th International Conference on Patient- and Family-Centered Care
More than 800 participants, including over 200 patient and family advisors, gathered in Baltimore in June 2018 for IPFCC’s 8th International Conference They came from the U.S., Canada, the Netherlands, South Korea, and several other countries. Plenary presentations, breakout sessions, and posters provided both inspiration and practical strategies related to the Conference’s theme of promoting health equity and reducing disparities. Leadership support was provided by The Armstrong Institute for Patient Safety and Quality, Johns Hopkins Medicine.
Strengthening Diversity in Research
In 2017, IPFCC received a Patient-Centered Outcomes Research Institute (PCORI®) Eugene Washington PCORI Engagement Award to support two major efforts: (1) Programming at IPFCC’s 8th International Conference on Patient- and Family-Centered Care: Promoting Health Equity and Reducing Disparities held in Baltimore, MD in June 2018 (see above) and (2) Development of a “Knowledge to Action Guide” providing strategies and guidance for creating and sustaining partnerships between researchers and individuals from diverse and under-represented communities. The Guide is based on an extensive literature review, consultation from an Expert Advisory Panel, interviews with researchers and diverse partners, and site visits to three exemplary programs.
Strategically Advancing Patient and Family Advisory Councils
in New York State Hospitals
A 2018 NYSHealth-funded report by IPFCC addresses gaps in knowledge about PFACs. While focusing on New York, the research findings documenting the landscape of hospital-based PFACs, as well as their prevalence and variation in characteristics, have broader application. The report also describes PFACs' performance and impact on hospital strategy and operations and correlation with experience of care and safety outcomes.

The Transforming Clinical Practice Initiative (TCPI) aims to help practices improve health outcomes, reduce unnecessary costs and improve patient experience. Person and Family Engagement (PFE) is a key strategy for ensuring widespread transformation in ambulatory care. IPFCC provides PFE technical assistance through the Patient Centered Care Collaborative (PCPCC) and the American College of Physicians (ACP) to this initiative. Six PFE metrics (shared decision making, e-tool use, medication management, patient activation, health literacy and patient family advisory councils) are areas of transformation. IPFCC’s technical assistance has included webinars, tools, and individual consultation to ambulatory practices implementing PFE metrics.
Hospital Innovation Improvement Networks
Since fall 2016, IPFCC has served as a subcontractor to the American Institutes for Research as part of the Patient and Family Engagement Support Contractor team supporting CMS’s Hospital Innovation Improvement Networks (HIINs). Systematic use of evidence-based patient and family engagement (PFE) best practices is fostered through coordinated technical assistance. IPFCC’s role includes developing tools; contributing content for learning events; developing training and implementation materials; serving as faculty for webinars and other learning events; and providing virtual and in-person TA to the HIINs and their member hospitals.
PCOR Translational Center
The Patient-Centered Outcomes Research Translation Center was created in 2016 to develop and publicly release findings of PCORI-funded studies in a manner that is accessible to everyone—the general public and clinicians and other health care professionals. The American Institutes for Research leads this Center and established a Technical Expert Panel (TEP) to provide input into key activities of the Translation Center. IPFCC has been a member of this TEP since 2016.

Individual and Family Engagement in the Medicaid Population
IPFCC prepared an issue brief: Individual and Family Engagement in the Medicaid Population: Emerging Best Practices and Recommendations (2014), sponsored by the Robert Wood Johnson Foundation's State Quality and Value Strategies program. The brief outlines best practices and suggested recommendations and strategies to support enhanced individual and family engagement efforts by Medicaid agencies, their staff, and organizations serving these populations.
IPFCC conducted a targeted literature review and a series of in-depth interviews, interviewing more than 50 individuals across the nation, including policy specialists, health care providers, engagement experts, and individuals and family members receiving Medicaid support. A small steering committee representing these perspectives helped guide the development of the report. The report and related resources including a summary of the methodology, bibliography, comprehensive summary of 50 interviews, and other resources are can be found at Engagement Strategies for the Medicaid Population.

Bev Johnson, IPFCC President & CEO, served on the Selection Committee for the American Hospital Association-McKesson Quest for Quality Prize


With the support of the Rothschild Foundation, IPFCC developed multimedia resource materials on partnering with patients, residents of long-term care facilities, and families to improve care, programming, and health care design. These resources are intended to be transformative, capturing the interest and sparking the creativity and commitment of leaders to encourage and support partnerships across the continuum of care.
Partnering with Patients, Residents, and Families: A Resource for Leaders of Hospitals, Ambulatory Care Settings, and Long-Term Care Communities, is a timely and comprehensive guide that shows how partnerships with patients, residents living in long-term care communities, and families have been essential to organizational change in health care settings across the continuum of care. It provides a framework for senior leaders to create and sustain effective partnerships and offers specific steps that leaders can take to develop partnerships to redesign and improve health care. Best practices from over 130 exemplary organizations provide concrete and real-world examples. Several practical tools and a listing of written, audiovisual, and online resources are included.
Partnerships with Patients, Residents, and Families: Leading the Journey, is a 20-minute video that highlights the accomplishments and ongoing activities of key leaders who have created exemplary partnerships in two health care organizations representing very different types of care settings—acute and long-term, urban and rural, and academic and community. The video captures the experiences of leaders in these organizations and shares their insights regarding the benefits of collaborating with patient, resident, and family advisors.
IPFCC is grateful to the Hulda B. & Maurice L. Rothschild Foundation for their support of both the guide and video. These resources are available for purchase in IPFCC's Bookstore.

In 2013, the American Hospital Association asked IPFCC to join an Expert Panel to develop a major national survey of hospitals to learn the current nature and extent of hospital efforts to improve patient and family engagement in health care. This was a collaborative initiative with the Health Research and Education Trust and the Gordon and Betty Moore Foundation.

IPFCC participated on a team, led by the American Institutes for Research, for an Agency for Healthcare Research and Quality (AHRQ) funded multi-year initiative to develop, evaluate, and implement a guide to promote patient and family engagement in hospital settings. Other organizations in this collaborative endeavor included, Consumers Advancing Patient Safety, the Joint Commission, the Health Research & Educational Trust, Planetree, the Maryland Patient Safety Center, Aurora Health Care, and Emory University Hospital.
In 2013, AHRQ released its Guide to Patient and Family Engagement in Hospital Safety and Quality. This online resource provides four evidence-based strategies for hospitals to engage patients and families in their care. These field-tested strategies can help make care better and safer by bridging the communication gaps among patients and families and their health care providers.
IPFCC collaborated with the Committee on Hospital Care of the American Academy of Pediatrics (AAP) in releasing the Patient- and Family-Centered Care and the Pediatrician's Role (2012). This revised AAP policy statement, co-written by Jerrold Eichner, MD, FAAP, Chair of the AAP Committee on Hospital Care 2007-2011, and Beverley Johnson, IPFCC's President and CEO, provided recommendations to promote patient- and family-centered care "throughout the health care system, including education of professionals, health care systems planning and facility design, and research."
The Academy first adopted a policy statement on Family-Centered Care and the Pediatrician's Role in 2003, and reaffirmed it in May 2007. An important difference in this 2012 policy statement is that the term family-centered care is replaced with the term "patient- and family-centered care," to "more explicitly capture the importance of engaging the family and the patient in a developmentally supportive manner as essential members of the health care team." This term recognizes that the "family is the child's primary source of strength and support and that the child's and the family's perspectives and information are important in clinical decision-making." This revised policy statement "specifically defines the expectation of patient- and family-centered care," citing research that indicates that patient- and family-centered care results in improved quality of care and patient safety, reduced health care costs, more effective use of health care resources, improved experience of care, and improved satisfaction for the patient, family, staff, and pediatrician.
IPFCC staff served as faculty to the NIC/Q 2009 Quality Improvement Collaborative of the Vermont Oxford Network (VON), which ran through December 2010. VON is an international organization committed to improving quality and safety in medical care for newborn infants and their families through education, research, and quality improvement. Multidisciplinary teams from 53 hospitals and several state-wide organizations worked with faculty to fulfill the Collaborative's vision: "To be an inclusive Community of Practice that supports the pursuit of shared goals for improvement and the provision of exemplary care for all newborn infants and their families." Family involvement in quality improvement is an integral part of VON initiatives: VON had a family member on its Advisory Board, a family member served on the core faculty team, and families were active participants on the majority of improvement teams.
From 1998 through 2005, IPFCC staff served as faculty and consultants for three quality improvement projects for VON.

IPFCC served as faculty for Team Up for Health, a California HealthCare Foundation initiative to develop partnerships with patients and families to advance the practice of self-management support (SMS) in six clinics throughout California, particularly those in underserved communities. Patients, families, staff, and physicians collaborated to improve educational resources to support active patient and family involvement in SMS, expand the use of information technology and social marketing, create linkages with community resources, and redesign clinic processes and workflow.

Between 2003-2009, IPFCC provided training and technical assistance for advancing patient- and family-centered care and facilitating the development of partnerships with patients and families in selected military hospitals and clinics worldwide, working on-site in more than 23 military treatment facilities in Europe and across the United States. In 2009, IPFCC worked with the United States Department of Veterans Affairs, providing training and technical assistance to nine medical centers and their affiliated clinics in VISN 7—which serves South Carolina, Georgia, and Alabama—to advance the practice of patient- and family-centered care.

In 2008, with funding support from the California HealthCare Foundation, IPFCC published Partnering with Patients and Families to Design a Patient- and Family-Centered Health Care System: Recommendations and Promising Practices. This publication builds upon the deliberations and key recommendations that emerged from the 2006 meeting convened by IPFCC in collaboration with the Institute for Healthcare Improvement and funded by the Robert Wood Johnson Foundation. Examples of best practices drawn from hospitals, ambulatory programs, medical and nursing schools, funders of health care, patient- and family-led organizations, and other health care entities are highlighted.
IPFCC's President and CEO, Bev Johnson, participated in the 2008 American Board of Internal Medicine (ABIM) Foundation Forum . The ABIM hosts an annual invitation-only meeting for health care leaderFrom Rhetoric to Reality: Achieving Patient-Centered Cares and key stakeholders to address an important, cross-cutting topic of shared concern. Unique to the 2008 meeting, the ABIM invited a group of patients and caregivers to share their stories.
Also in 2008, the ABIM convened a task force to assess teamwork—identified by the ABIM as one of the most critical competencies in internal medicine. IPFCC's then Director of Special Projects, Julie Moretz, (now Associate Vice Chancellor for Patient- and Family-Centered Care at the University of Arkansas for Medical Sciences) participated in the 10-member working group comprised of both physicians and non-physicians.

IPFCC staff members served on a leadership faculty team from 2005-2008 with the Institute for Healthcare Improvement (IHI), Rush Medical College and John H. Stroger Hospital of Cook County, White Mountain Research Associates, and the MacColl Institute with funding from the Robert Wood Johnson Foundation. The purpose of the Quality Allies project was to create a Collaborative Self-Management Support Learning Network aimed at improving chronic illness care. Patient and family leaders served on the National Advisory Council and on the core faculty team. Twenty teams participated in the collaborative and each team included patients and families as active members. This initiative was re-named New Health Partnerships: Improving Care by Engaging Patients.
This initiative was followed by a two-year project to create and support a virtual learning collaborative among nine teams and develop a virtual community.