The University of Cincinnati Department of Family and Community Medicine and The Christ Hospital Family Medicine Center

The University of Cincinnati Department of Family and Community Medicine was awarded a 5-year, $1.75 million, grant from HHS/HRSA, in partnership with the Family Medicine Residency, Faculty, and Residency Clinic. The purpose of the grant was to help residents and fellows become more effective “change agents” in primary care practices. Foundational to the grant project was the belief that true practice transformation requires meaningful input from patients and families.
The Christ Hospital Family Medicine Center (FMC) was selected as the first pilot in the grant initiative. Located in Cincinnati, Ohio, the FMC has a total of 9 faculty providers and 26 resident physicians who provide full-spectrum primary care for approximately 7000 patients, with 23,000 annual visits. The practice, a certified patient-centered medical home, is 60% Medicare/Medicaid; the remainder is private insurance.
To drive quality improvement initiatives for the FMC, the grant team helped launch a PFAC there in 2016. A physician champion and a staff champion were recruited early in the process to ensure credibility for the PFAC. Providers and staff identified potential patient and family advisors. In the second year, PFAC recruitment focused on expanding the group of advisors so they more accurately represented the diverse racial and socioeconomic population of the FMC.
The PFAC meets monthly with Patient and Family Advisors (PFAs), Family Medicine residents, office staff, and the medical director. In 2018, the PFAC had 30 members; 18 of them were PFAs, including 5 eAdvisors. PFAs share their stories, help identify quality improvement projects, provide iterative feedback, weigh in on clinic issues, review and edit educational materials, and bring concerns/topics of interest to the group for discussion.
PFAs value their participation on the PFAC and have shared comments like, “It’s great to be a part of something that is helping making a tangible change,” and “Sharing personal stories at the start of the year helped me understand where each member’s perspective is built from.”

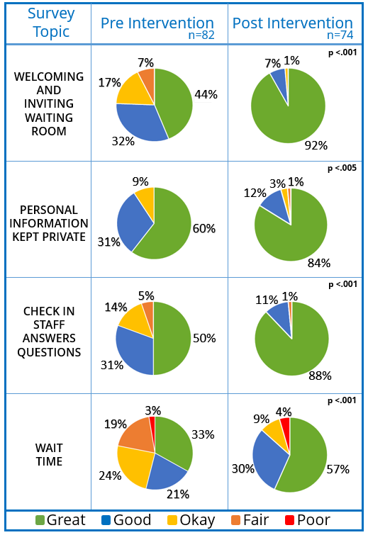
In 2016-2017, the focus of PFAC initiatives was patient experience, specifically, the waiting room. A complete redesign, with PFA input, led to measurable patient perception improvements in accessibility, wait times, and functionality of the front office.
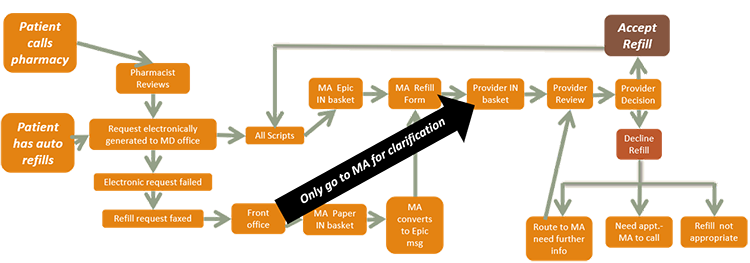
In 2017-2018, the focus was improving direct care through the medication refill process. A process map was developed to diagram the steps necessary for a “simple” refill; refills are now completed in roughly half the time. All PFAC initiatives utilize established QI techniques, including rapid cycle QI, and outcomes are measured and reported at every step.
Because of the success with The Christ Hospital FMC, another PFAC was created at a Community Underserved Partner Site in fall 2018. In the fall of 2019, the grant initiative will mentor two additional PFACs.