What is patient- and family-centered care?
New Resources
IPFCC developed this resource to assist health care organizations in increasing the diversity of PFAC members and expanding the role of PFAs in diversity, equity, and inclusion efforts.
IPFCC completed two PCORI-funded engagement projects focused on the impact of restricting family presence during COVID-19 in long-term care settings and hospitals. Four new resources were developed and are available for download.
IPFCC's 2023 Highlights
IPFCC is excited to share the 2023 Highlights of our work with you:
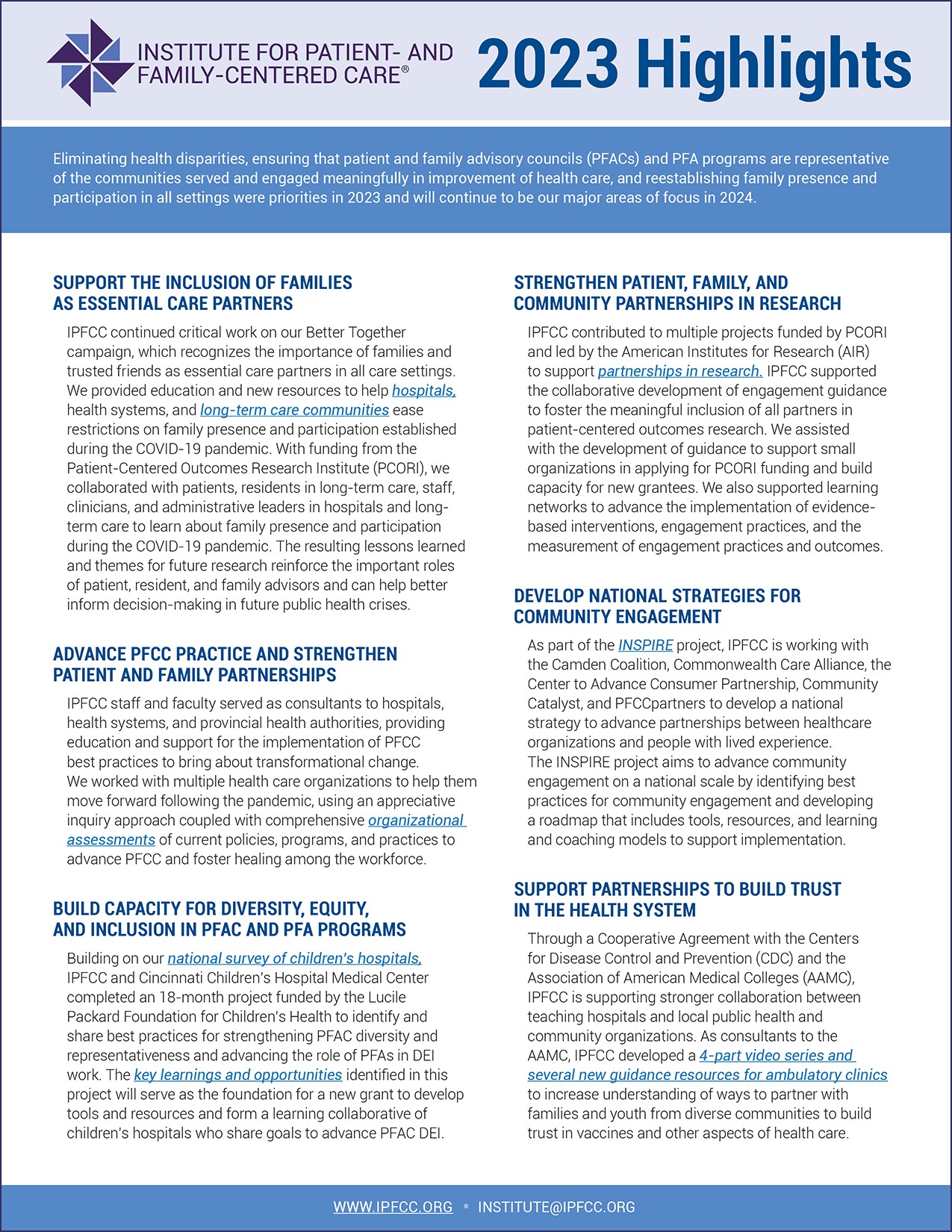
- Eliminating health disparities;
- Ensuring that patient and family advisory councils (PFACs) and PFA programs are representative of the communities served and engaged meaningfully in improvement of health care; and
- Reestablishing family presence and participation in all settings.
These 2023 priorities will continue to be major areas of focus in 2024.
Join Our Online Community
Thanks to our PFCC.Connect Pinwheel Sponsors, PFCC.Connect is IPFCC's FREE online learning community for anyone interested in connecting with, learning from, and sharing ideas with others.
Stay Updated with IPFCC
Stay connected with IPFCC’s latest news, events, and resources! The Newsletter will make it easier for you to learn about and register for IPFCC events. Register for the monthly newsletter, and more.